Behavioral Research Program
A Comprehensive Program for Behavioral Research in Cancer Prevention and Control
Up to 50% of cancer deaths are attributable to behaviors such as tobacco use, unhealthy diet, lack of physical activity, ultraviolet (UV) exposure, and alcohol consumption. Undeniably, behavior — including communication — is an important factor across the cancer control continuum. Social media users post information — sometimes inaccurate information — about cancer causes and treatments, read by thousands. Oncologists communicate with patients and families and make treatment and palliative care decisions, and radiologists make judgments based on training and prior experience when evaluating mammograms. Lawmakers design policies that influence behavior, such as laws that prohibit indoor tanning among youths and smoking in public places and workplaces. Patients decide whether to engage in genetic testing to better understand their cancer risk. Indeed, the human experience can play a part in many cancer outcomes. Stress can accelerate tumorigenesis; cancer treatment can diminish cognitive abilities; cancer can accelerate the aging process; and anticipated emotions can drive big decisions, such as enrolling in a clinical trial.
Recognizing the impact of human behavior on cancer morbidity, mortality, and survivorship, NCI established the Behavioral Research Program (BRP) in 1998. Since then, BRP has built a large and diverse grants portfolio in behavioral research related to cancer (nearly 300 grants awarded totaling almost $200 million in FY 2020). The portfolio features grants on a wide range of topics, including interventions to address tobacco initiation and cessation in high-risk groups, such as youths, cancer patients, and people living with HIV; innovative applications of mobile health technology to manage cancer symptoms; and state-of-the-art programs to promote physical activity in cancer survivors. Many grants focus on health drivers by addressing cancer prevalence and control in traditionally underrepresented subpopulations.
BRP has prioritized the support of data and research tools to advance the integration of behavioral science and cancer control and to facilitate the research pursuits of our extramural community. These tools include the Health Information National Trends Survey (HINTS), a nationally representative survey of engagement with health information; the Family Life, Activity, Sleep, Health, and Eating (FLASHE) survey, which assesses health behaviors and predictors in parent-adolescent dyads; the Grid-Enabled Measures (GEM) portal, a collaborative tool to help groups reach consensus about best measures in disparate areas of cancer control; the Classification of Laws Associated with School Students (CLASS) data set, which collects policy data related to obesogenic factors affecting youth, such as physical activity requirements; and the Tobacco Use Supplement to the Current Population Survey (TUS-CPS), which tracks tobacco use behaviors, attitudes, and policies across the US.
BRP uses insights from basic communications science and basic behavioral science to inform cancer prevention and control, including the application of (1) communication “best practices” in the design of anti-tobacco messaging; (2) basic research on decision-making to understand and improve palliative care decisions; (3) research on stigma to understand and narrow disparities in pain management; (4) cognitive science research to determine how best to assess the effects of chemotherapy on cognitive functioning; and (5) research on nutrition, physical activity or sedentary behaviors, sleep behavior, and the built environment, to elucidate the links among obesity, energy balance, and cancer prevention. The program also takes a full lifespan approach — ranging from research on predictors of obesity and the use of electronic nicotine delivery systems (ENDS) in children to predictors of frailty and cognitive decline in older cancer survivors. A key priority is to take a systemic, multilevel approach, because behaviors are influenced by factors at many levels — from individual factors, like emotions, to sociocultural factors, such as structural racism and the built environment. In collaboration with other institutes and centers (ICs) and offices within the National Institutes of Health (NIH), BRP has advanced innovative research methods, such as integrative data analysis, intensive longitudinal assessments, and natural experiments, and has employed innovative methods, such as NCI - Cancer Research U.K. (CRUK) “Sandpit” idea labs and summer workshops, to build new areas of research and to facilitate the career development of early-stage investigators.
BRP research needs to be particularly nimble and responsive to national and international developments. When the FDA was provided the authority to regulate tobacco products in 2009, BRP supported critical research efforts to help inform the development of new policies, and when menu labeling was mandated in 2008, BRP supported research to assess the effects of labels on dietary choices. The COVID-19 pandemic, the nation’s reckoning with structural racism, public skepticism about the value of science (combined with the spread of health misinformation), and even the increasing threat of climate change on human health will all influence behavioral factors along the cancer control continuum. The rapid increase in cancer survivors due in part to promising developments in cancer therapeutics necessitates a focus on helping survivors engage in behaviors that enhance longevity and that minimize the risk of recurrence and secondary cancers. With a concerted effort, it should be possible to reduce the number of preventable cancers and to make a lasting contribution to population health.
Basic Biobehavioral and Psychological Sciences Branch: Brain, Behavior, and Cancer Control
Use-inspired basic research is fundamental to understanding human behaviors, social context, decision-making, and clinical practices. The Basic Biobehavioral and Psychological Sciences Branch (BBPSB) supports experimental studies involving humans or animals and observational and clinical studies that broaden our knowledge of cognitive, affective, perceptual, and sensory processes related to cancer etiology, prevention, screening, detection, diagnosis, treatment, and survivorship.
Decision Science, Affect, and Emotion
BBPSB has endeavored to understand how individuals make health-related decisions about cancer. Over the last 20 years, BBPSB has supported research to develop decision support tools (e.g., electronic decision aids) and research to understand how individuals apply heuristics and biases to health-related decisions (e.g., understanding numeric risk estimates). Recently, BBPSB developed a Cancer Moonshot initiative to improve risk communications and decision-making for individuals and families with an inherited susceptibility to cancer.
In 2011, BBPSB articulated the need to support basic research on the phenomenological nature of affect to advance understanding of how emotion influences cancer control. Three workshops led to a white paper, NCI and trans-NIH funding opportunities, and the Society for Affective Science inaugural meeting. In 2015, BBPSB convened four meetings of affective/decision scientists and palliative care researchers/practitioners and developed a conceptual model of affective prediction in palliative care (published in 2019).
Interoception and Perception
Interoception is the perception and integration of autonomic, hormonal, visceral, and immunological homeostatic signals that collectively describe the body’s physiological state. Fundamental knowledge of interoception can be leveraged to understand aspects of cancer control, such as the role of hunger and satiation perception in obesity, the perception of pain and other symptoms, individual differences in patient-reported outcomes, and treatment adherence. BBPSB established the Interoception Research Network in 2019 to promote discussion and collaboration among interoception experts.
Detecting and diagnosing cancer often relies on humans interpreting complex medical images, such as mammograms or pathology slides. In an era of rapidly advancing imaging technologies, the role of the human observer remains critical. To improve diagnostic accuracy, we must understand the perceptual and cognitive mechanisms underlying medical image perception. BBSPB convened an agenda-setting workshop (2014) and a think tank (2019), which led to funding opportunities in collaboration with the National Institute for Biomedical Imaging and Bioengineering (NIBIB) and the NSF. Further, BBPSB sponsored mobile perception laboratories at radiological meetings and launched a platform for online medical image perception experiments to connect researchers and clinical diagnosticians.
Multimorbidity, Aging, Cognitive Impairment, and Pain
BBPSB continues to expand its research portfolio in the areas of multimorbidity, accelerated aging, cancer-related cognitive impairment, and cancer pain inequities to improve survivorship and extend health span. Cancer survivors are more likely than those without cancer to experience multimorbidities and premature mortality, and more than 50% of cancer survivors experience overweight or obesity. BBPSB established the Perspectives on Cancer and Aging: The Arti Hurria Memorial Webinar Series, in partnership with EGRP, to honor the late Arti Hurria, MD, a pioneer in the fields of geriatrics and oncology, a BBPSB grantee, and servant-based leader, collaborator, and mentor. In addition, the Cancer and Accelerated Aging initiative, started in 2017 with EGRP, convened think tank meetings to understand how best to measure aging in cancer populations and identify strategies to prevent, ameliorate, or rehabilitate the aging-related consequences of cancer.
A significant proportion of non-central nervous system cancer survivors report mild cognitive impairment at diagnosis, during treatment, and for some, for years after treatment completion. Recognizing the opportunity to leverage cognitive neuroscience to improve the assessment of cancer-related cognitive impairment (CRCI), BBPSB published a commentary in Trends In Neurosciences to encourage research through grant and contract mechanisms and created the CRCI-Cognitive Science Network to encourage transdisciplinary collaboration.
“If you want to go fast, go alone. If you want to go far, go together.”Proverb shared by Dr. Arti Hurria, Founding Chair, Cancer and Accelerated Aging: Advancing Research for Healthier Survivors
Biobehavioral Mechanisms of Cancer Progression
BBPSB has led NCI’s investment in discovering cancer-relevant molecular pathways and networks regulated by social, behavioral, or psychological factors. Over the last 20 years, the branch convened subject-matter experts to inform scientific agenda-setting, sponsored roundtables, symposia, and workshops, published seminal field-shaping perspectives, and cultivated a preclinical and clinical portfolio of research project grants. BBPSB founded the NCI Network on Biobehavioral Pathways in Cancer, a collaborative research consortium comprising scientists with expertise in molecular biology, biobehavioral sciences, preclinical and translational medicine, and clinical oncology. Between 2010 and 2018, requests for proposals released by Leidos Biomedical, Inc. resulted in 14 subcontract awards that fulfilled the network’s mission and contributed to a feature in Science magazine.
Health Behaviors Research Branch: The Promise of Cancer Prevention and Control Through Behavior Change
Imagine a regimen that could prevent up to one-half of all cancer deaths; such a discovery would galvanize the world of cancer prevention and treatment.
We have at hand such a “magic formula,” though not in pill form. As stated before, up to 50% of cancer deaths are believed to be attributable to unhealthy behaviors and could be prevented. While tobacco use is the most important modifiable risk factor, other behavioral risk factors such as obesity, lack of physical activity, unhealthy diets, alcohol use, and UV radiation exposure, account for a large proportion of preventable cancer deaths (Lippman et al).
“Effective cancer prevention requires evidence-based personal and population actions.”Lippman et al, 2018
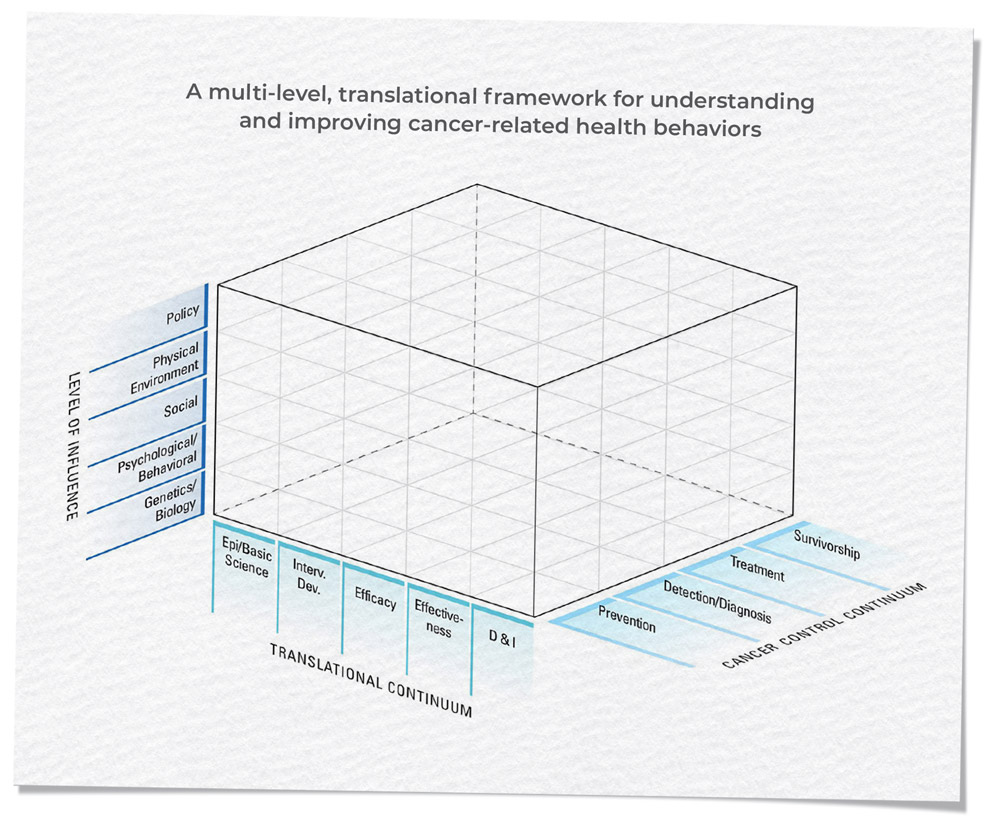
The Health Behaviors Research Branch (HBRB) has made significant progress over the past 20 years in supporting and catalyzing research to develop, test, and implement effective strategies to improve cancer risk behaviors and to evaluate programs, policies, and environments that influence such behaviors. Through this research, the branch has discovered that adopting and maintaining healthy behaviors requires a deep understanding of the complex, multilevel array of influences on human behavior. HBRB-supported research spans multiple levels of influence, all phases of the translational spectrum, and all aspects of the cancer control continuum, as illustrated by the HBRB strategic plan and accompanying multilevel framework.
Advancing the Science of Energy Balance, Obesity, Diet, Physical Activity, and Cancer
Since the early 2000s, HBRB has worked to advance our understanding of obesity, poor diets, and low levels of physical activity; identify the relationship of these risk factors to cancer incidence, progression, and outcomes; and devise more effective strategies to mitigate their adverse effects. The branch created the FLASHE survey to assess health behaviors and predictors in parent–adolescent dyads. It established the TREC consortium, which focused on elucidating the relationships between energy balance, body weight, and cancer, and laid the groundwork for characterizing how energy balance, obesity, diet, and physical activity influence cancer incidence and treatment outcomes through biological and behavioral pathways. DCCPS was a foundational member and continues to be a major supporter of the National Collaborative on Childhood Obesity Research (NCCOR), a public-private collaboration among three federal agencies (NIH, CDC, and the USDA) and the Robert Wood Johnson Foundation, aimed at reversing the epidemic of overweight and obesity among US youths. These and other projects formed the foundation for the branch’s current work and demonstrate the benefits of transdisciplinary partnerships in advancing the science of energy balance, obesity, and cancer.
This work has evolved to incorporate new concepts, such as precision prevention in the areas of nutrition and weight loss, while also promoting broader environmental and policy approaches to cancer prevention and control. Current projects in the area of precision prevention include the Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) Core Measures and Trans-NIH Consortium of Lifestyle Weight Loss Interventions, both of which aim to identify predictors of successful weight loss and to incorporate information on genetic, psychosocial, behavioral, biological, and environmental factors into predictive profiles to enable more precise and, ultimately, more effective weight loss interventions.
HBRB’s support for environmental, geospatial, and policy research represents a broader direction for our work. The branch is investigating the impact of policy and social determinants of health in such projects as the trans-NIH FOA on time-sensitive obesity policies and the CLASS project. HBRB has promoted the use of translational frameworks for intervention development and testing (e.g., Obesity-Related Behavioral Intervention Trials [ORBIT] model), stimulated advances in geospatial and environmental measurement and methods, and led efforts in methodological innovation in natural experiments (e.g., Pathways to Prevention [P2P] Methods workshop program).
HBRB is tackling problems in cancer prevention and control at the intersection of climate change, health inequities, and advances in research that allow for targeting multilevel interventions with both individual- and policy-level strategies. Future directions will include the integration of guideline-based health behavior recommendations into care for cancer survivors and the development of research networks that support the testing of multilevel interventions by embedding studies on individual-level, obesity-related behavior change within natural experiments of communities adopting obesity prevention and control policies.
Investigating Emerging Cancer Risk Factors
HBRB aims to better understand and develop behavioral and policy-focused interventions in emerging areas, such as alcohol and sleep, by leveraging lessons learned in other areas, like tobacco control. The branch has led and participated in symposia and panels at major meetings; organized an NCI-sponsored workshop on alcohol and cancer; and developed and participated in an NCI-National Institute on Alcohol Abuse and Alcoholism (NIAAA) FOA. The workshop led to a white paper authored by leading researchers on alcohol as a target for cancer prevention and control. The branch is actively engaged in efforts to address prevention of alcohol-related cancers and to understand the synergistic interactions of alcohol and tobacco across the cancer control continuum.
Recognizing the transdisciplinary nature of sleep and circadian dysfunction research, HBRB is collaborating with staff in other DCCPS branches (e.g., BBPSB), programs (e.g., EGRP), NCI divisions, and NIH institutes and centers to develop a scientific interest group, participate in several trans-NIH FOAs, and create a “sleep team” of NCI and extramural experts to define future research needs.
Over the past two decades, HBRB has made significant strides in addressing the challenging task of improving cancer-related risk behaviors and in creating a strong foundation for realizing HBRB’s vision of a world in which individuals, families, and communities engage in healthy lifestyles to prevent cancer, improve treatment outcomes, and optimize health and well-being.
Health Communication and Informatics Research Branch: Keeping Pace with an Evolving Communication Landscape
Health communication science has been a priority for NCI for over two decades, since its identification as an “extraordinary opportunity for investment” in the NCI Budget Proposal for FY 2001. The budget proposal stated, “… there is a need for a public institution such as NCI to provide leadership in the cancer communications arena; the broad and reasoned perspective that NCI brings to patients and healthcare providers alike is essential to successfully implement communications strategies to reduce the cancer burden.” The Health Communication and Informatics Research Branch (HCIRB) — the only research branch at NIH focused on communication research — continues to lead efforts to realize the promise of this investment in a rapidly changing communication landscape.
Health Communication Surveillance: HINTS
NCI’s HINTS, the only nationally representative health communication surveillance vehicle, has been collecting data on trends in cancer communication and information technology (IT) since 2003. Across 14 administrations, HINTS has surveyed more than 55,000 American adults, tracking profound shifts in the communication landscape. HINTS has a robust community of over 10,000 data users, who have published more than 600 peer-reviewed papers using publicly accessible HINTS data. To date, the HINTS program has also published 46 HINTS Briefs, which provide a snapshot of published HINTS research on such topics as trust in health information resources, tobacco risk perceptions, cancer knowledge and awareness, and the information support needs of cancer survivors.
Social Media and Health
The communication landscape has been transformed by the rise of social media over the past two decades, posing new research questions for cancer communication. HCIRB has been at the forefront of research at the intersection of social media and health. The branch collaborated with NIDA and NIAAA on an RFA in 2013 titled “Using Social Media to Understand and Address Substance Use and Addiction,” which resulted in 11 research projects that leveraged social media to advance understanding of tobacco, alcohol, and illicit drug use and test-related interventions. HCIRB continues to support social media research through the “Innovative Approaches to Studying Cancer Communication in the New Information Ecosystem” program announcements (PAs), which have funded 13 grants since 2016. Funded grants have assessed the impact of health-related Facebook advertisements and monitored tobacco-related communication on Twitter, for example.
As the amount of misinformation circulating on social media became more apparent, HCIRB convened a multidisciplinary working group in 2018 to develop a research agenda for cancer-related misinformation on social media. The meeting led to the publication of high-profile editorials in the Journal of the American Medical Association (Chou et al.) and the American Journal of Preventive Medicine (Southwell et al.), outlining priorities and key considerations for research and practice. These efforts were followed by an NCI-sponsored special issue of the American Journal of Public Health in October 2020, which addressed critical issues related to online misinformation, including antivaccine messaging, bots, and the impact of content-moderation policies.
Patient-Centered Communication
In response to the evolving communication landscape in healthcare, HCIRB also focuses on promoting patient-centered communication, including research on health literacy. In 2007, NCI commissioned a monograph Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering, which focused on optimizing the communications process between patients and families and healthcare delivery teams. For more than a decade, the monograph’s conceptual framework has served as a cornerstone for research on patient-centered cancer communication.
HCIRB participated in the trans-NIH “Understanding and Promoting Health Literacy” PA from 2004 to 2016, which resulted in 25 funded grants. More recently, HCIRB partnered with the National Institute of Nursing Research to support health literacy research in specific domains, including advanced illness and end-of-life communication, through the “End-of-Life and Palliative Care Health Literacy” funding opportunity.
HCIRB has also been involved with efforts to leverage technology in support of patient-centered cancer care. HCIRB contributed to the 2016 President’s Cancer Panel report “Improving Cancer-Related Outcomes With Connected Health,” and collaborates with the NSF on the Smart and Connected Health interagency funding opportunity, which supports interdisciplinary high-risk, high-reward technology-based solutions coupled with biobehavioral health research. HCIRB’s recent contributions to NCI’s Telehealth in Cancer Care initiatives and NIH’s COVID-19 response demonstrate continued commitment to ensuring that communication research remains current as major shifts in the health, social, and technological landscape unfold.
At this pivotal juncture, there is a need for a public institution such as NCI to provide leadership in the cancer communications arena; the broad and reasoned perspective that NCI brings to patients and healthcare providers alike is essential to successfully implement communications strategies to reduce the cancer burden.”From the NCI 2001 Annual Plan
Tobacco Control Research Branch: Toward a Tobacco-Free World
Tobacco research has been integral to NCI research efforts for many years. In the 1950s, NCI scientists conducted studies and developed research methods that documented cigarette smoking as the primary causal agent underlying the dramatic rise in lung cancer seen in the 20th century. In the decades that followed, NCI funded and conducted research to prevent and control tobacco use. These efforts have contributed to the nation’s tremendous progress in reducing tobacco use and tobacco-related disease.
The Tobacco Control Research Branch (TCRB) continues to build on this storied history. TCRB leads and collaborates on research and disseminates evidence-based findings to prevent, treat, and control tobacco use to create a world free of tobacco use and related cancer and suffering. A key research area involves tobacco-related disparities, because not all groups have experienced the same degree of benefit. TCRB has supported research demonstrating that a powerful lever of behavior change involves the conversion of social, economic, and policy environments that support tobacco use into those that support tobacco-free norms. TCRB also plays a crucial role in the surveillance of tobacco use, provision of evidence-based cessation services to the public, and the synthesis and dissemination of research findings.
Tobacco Use Surveillance
NCI has sponsored the TUS-CPS, administered by the US Census Bureau, since 1992–1993. The survey is a key data source of national, state, and sub-state data on tobacco use behaviors, attitudes, and policies. TCRB scientists have created harmonized data files to enhance the survey’s usability across multiple time points and have linked the TUS-CPS to the National Death Index to create the Tobacco Longitudinal Mortality Study — the largest dataset linking tobacco use to mortality and to other morbidity outcomes.
Evidence-Based Cessation Services
TCRB staff members created and maintain the Smokefree.gov Initiative, a multimodal suite of digital interventions (e.g., websites, text message programs, mobile apps) that provides free, evidence-based cessation support to smokers interested in quitting. Through partnerships with FDA, CDC, VA, and other federal agency partners, the initiative provides assistance to a wide variety of populations.
Synthesizing Research Findings
NCI established its Tobacco Control Monograph series in 1991 and has since published 22 volumes, many of which have made seminal contributions to the literature. Monograph 13 (2001) established the deception inherent in the marketing of low-yield, low-tar cigarettes; Monograph 19 (2008) demonstrated the causal relationship between tobacco advertising and promotion and increased tobacco use; and Monograph 21 (2016), produced with the WHO, summarized the evidence that tobacco control interventions make sense from an economic and a public health perspective across the globe.
Addressing Key Challenges Now and in the Future
As TCRB looks to the future, new challenges lie ahead, such as the growth in ENDS use and changes in state and local laws regulating cannabis use that may be altering patterns of tobacco use among both youths and adults. Although developing technologies provide new opportunities to deliver tobacco cessation and prevention interventions, they have also enhanced the tobacco industry’s ability to promote tobacco use. The 2009 Family Smoking Prevention and Tobacco Control Act (Public Law 111-31) provided regulatory authority to FDA; this law has dramatically reshaped the US regulatory landscape and has generated a need for NCI-supported regulatory science to inform FDA. In addition, the entry into force of the WHO Framework Convention on Tobacco Control has unleashed a wave of new policy implementation across the globe. Today, many of the most informative research studies are those that compare the implementation of policies and programs across countries.
TCRB is addressing these and other challenges through its large and diverse grant portfolio, which includes targeted funding initiatives, such as those that are aimed at (1) stimulating scientific inquiry focused on innovative state- and local-level tobacco prevention and control policies to promote health equity (PAR 20-302/303) and (2) improving smoking cessation interventions to reduce tobacco use among people living with HIV, whose smoking rate far exceeds the population average. TCRB also participates in several funding initiatives to understand the patterns of ENDS use, their short- and long-term harms, and their potential benefits, such as NIH’s Tobacco Regulatory Science Program, a partnership between NIH and FDA to fund research to inform FDA’s regulatory authority.
“I call upon the entire medical and public health community to become involved in the fight against this Nation’s number one public health menace — cigarette smoking.”Dr. Samuel Broder, Former NCI Director
Former NCI Director Dr. Samuel Broder wrote in NCI Monograph 1 (1991), “I call upon the entire medical and public health community to become involved in the fight against this Nation’s number one public health menace — cigarette smoking.” This call to action still resonates. TCRB remains committed to funding cutting-edge research to inform efforts to eradicate tobacco use in the United States and around the world.
Footnotes
Lippman SM, et al. AACR white paper: shaping the future of cancer prevention – a roadmap for advancing science and public health. Cancer Prev Res (Phila). 2018 Dec;11(12):735–778.
Chou W-YS, et al. Addressing health-related misinformation on social media. JAMA. 2018 Dec 18;320(23):2417–2418.
Southwell BG, et al. Misinformation as a misunderstood challenge to public health. Am J Prev Med. 2019 Aug;57(2):282–285.
Continue To